While traditionally considered in the context of digestion alone, burgeoning research reveals that maintaining good gut health is crucial for overall well-being. The gut, often referred to as the second brain, is home to a complex ecosystem known as the gut microbiome, comprised of trillions of microorganisms. These inhabitants play a vital role not just in digestion but in regulating various bodily functions. From influencing mental health through the gut-brain axis to acting as a key player in our immune system, the gut exerts a far-reaching impact. Moreover, a healthy gut is integral to efficient metabolic functions, revealing its importance in weight management and the prevention of metabolic diseases. By understanding and nurturing gut health, we open doors to enhancing mental well-being, bolstering immunity, and achieving optimal metabolic health. Delve deeper to uncover the profound ways your gut influences your entire body and discover actionable tips for maintaining a healthy gut ecosystem.
Introduction to Gut Health
The human gut, or gastrointestinal tract, plays a crucial role far beyond the simple digestion of food. This extensive system, running from the mouth to the anus, is fundamental to overall health and well-being. A burgeoning body of research suggests that gut health is intricately linked to numerous bodily functions, emphasizing the importance of maintaining a balanced and healthy gut.
One of the most significant discoveries in recent years is the connection between gut health and overall well-being. Scientists now understand that the gut communicates with nearly every system in the body. This communication helps regulate various processes, including metabolism, immune function, and even mental health. Therefore, maintaining a healthy gut can have far-reaching implications for one’s holistic health.
The Importance of Gut Health
Gut health is determined by the balance and function of the gut microbiome — a complex community of trillions of microorganisms, including bacteria, viruses, fungi, and other microbes living in the digestive tract. According to Harvard Medical School, a healthy gut can enhance nutrient absorption, bolster immune defenses, and even aid in preventing chronic illnesses.
Conversely, an imbalance or dysbiosis in the gut microbiome has been linked to a host of health problems. These can range from digestive disorders like irritable bowel syndrome (IBS) to more systemic conditions such as type 2 diabetes, cardiovascular disease, and even certain cancers. Therefore, understanding and maintaining gut health is essential for preventing disease and promoting long-term wellness.
The Connection Between the Gut and Overall Well-Being
One of the most fascinating aspects of gut health is how it influences overall well-being. For instance, the gut is involved in the production of neurotransmitters — chemicals that transmit signals in the brain. Serotonin, commonly known as the ‘feel-good’ neurotransmitter, is primarily produced in the gut, with about 90% of the body’s serotonin being synthesized there.
This connection between the gut and the brain is part of what is known as the gut-brain axis. The gut-brain axis refers to the bidirectional communication between the central nervous system and the gut. Disruptions in this communication are increasingly being recognized as contributing factors to conditions such as anxiety and depression. Therefore, maintaining gut health can have profound implications for mental well-being.
A Brief Explanation of the Gut Microbiome
The term ‘gut microbiome’ refers to the collective genomes of the microorganisms residing in the gut. Each individual’s microbiome is unique and shaped by various factors, including diet, environment, genetics, and lifestyle. According to the National Institutes of Health (NIH), the gut microbiome plays essential roles in digesting food, absorbing nutrients, and protecting against harmful pathogens.
Diet enormously influences the composition and function of the gut microbiome. For example, a diet high in fiber-rich foods such as fruits, vegetables, and whole grains can promote the growth of beneficial bacteria. These bacteria, in turn, produce short-chain fatty acids (SCFAs) like butyrate, which have anti-inflammatory properties and contribute to gut health.
On the other hand, a diet high in processed foods, sugar, and fats can disrupt the balance of the microbiome, leading to dysbiosis. This imbalance is associated with various health issues, including inflammation, obesity, and metabolic syndrome. Hence, fostering a balanced gut microbiome is critical for sustaining health and preventing disease.
In conclusion, gut health is a cornerstone of overall well-being. The intricate relationship between the gut and various body systems underscores the importance of a balanced gut microbiome. Through mindful dietary choices, lifestyle changes, and a deeper understanding of this complex organ system, we can optimize our gut health and, by extension, our overall health.
The Gut-Brain Axis: Mental Health Connections
Understanding the Gut-Brain Axis
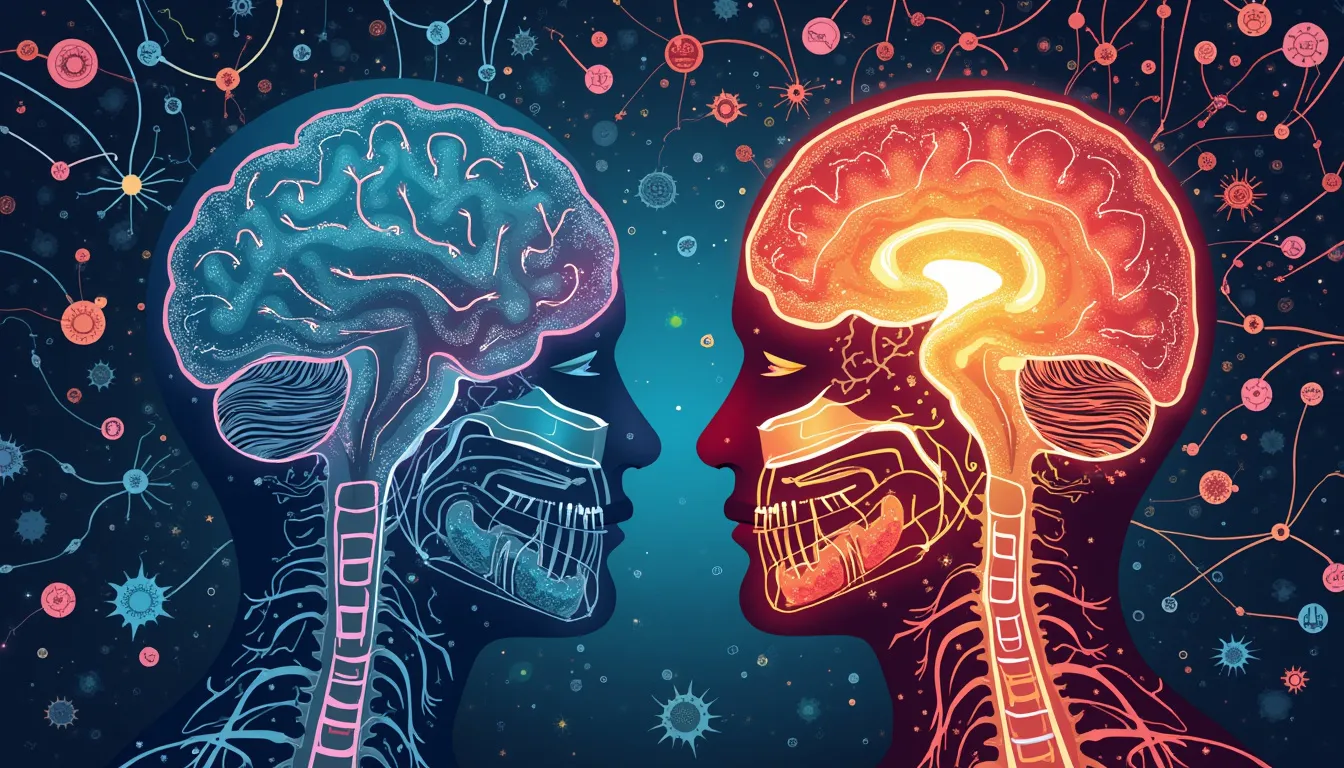
The gut-brain axis refers to the complex bidirectional communication network that links the gastrointestinal system and the central nervous system. This term encapsulates the intricate alliance between gut microbiota—the trillions of microorganisms residing in the digestive tract—and the brain. The gut is often dubbed the second brain due to its vast neural network, known as the enteric nervous system, which operates semi-independently from the brain and spinal cord. It plays a crucial role in managing gastrointestinal functions and has a significant impact on emotional and cognitive processes.
How Gut Health Impacts Mental Health and Cognitive Function
The relationship between gut health and mental well-being is profound and multifaceted. Various pathways facilitate communication between the gut and the brain, including the vagus nerve, immune system, and the production and regulation of neurotransmitters and metabolites.
1. **Vagus Nerve:** Serving as a major conduit between the gut and the brain, the vagus nerve transmits signals in both directions. Alterations in gut microbiota can influence vagal signals, potentially impacting brain functions related to mood and anxiety.
2. **Neurotransmitter Production:** The gut microbiota contribute to the production of essential neurotransmitters such as serotonin, dopamine, and gamma-aminobutyric acid (GABA). Approximately 90% of serotonin, a neurotransmitter pivotal in mood regulation, is synthesized in the gut.
3. **Inflammatory Responses:** Gut bacteria modulate the immune system, and imbalances can lead to chronic inflammation, contributing to mental health disorders.
4. **Metabolites:** Certain gut bacteria produce short-chain fatty acids (SCFAs) through the fermentation of dietary fibers. These SCFAs, including butyrate, play a role in maintaining the integrity of the blood-brain barrier and modulating neuroinflammation.
Recent Studies Linking Gut Bacteria to Mood Disorders and Mental Health Conditions
Emerging research underscores the influence of gut microbiota on mental health. Several studies have sought to unravel this complex interconnection:
1. **Depression and Anxiety:** A study published in the journal *Nature Microbiology* found that individuals with depression exhibited reduced levels of *Faecalibacterium* and *Coprococcus*, both of which are associated with anti-inflammatory properties and the production of SCFAs. Another study published in *General Psychiatry* reported that patients with anxiety disorders had an altered gut microbiome composition compared to healthy individuals, hinting at a potential therapeutic target for these disorders.
2. **Autism Spectrum Disorder (ASD):** A review in *Frontiers in Cellular Neuroscience* highlighted various animal and preliminary human studies demonstrating gut microbiota differences in individuals with ASD. Modulating gut bacteria through probiotics or diet has shown potential in alleviating behavioral symptoms in some cases.
3. **Cognitive Function:** Research published in *Frontiers in Aging Neuroscience* examined the correlation between gut microbiota diversity and cognitive performance in older adults. The study suggested that higher gut microbiota diversity was associated with better cognitive functions, indicating that maintaining gut health could be crucial for preventing cognitive decline in aging populations.
4. **Bipolar Disorder and Schizophrenia:** An analysis in *Current Psychiatry Reports* pointed to distinct gut microbiome profiles in patients with bipolar disorder and schizophrenia. These findings suggest that gut health interventions could complement traditional psychiatric treatments.
In conclusion, the gut-brain axis underscores the critical role of gut health in influencing mental health and cognitive functions. As research advances, we may see more targeted therapies to modulate the gut microbiome as a means to mitigate and manage mental health conditions. Understanding and nurturing the health of our gut could, therefore, be a crucial step towards optimal mental well-being.
The Immune System: Gut as a Key Player
The relationship between the gut and the immune system is intricate and profound, offering essential insights into how our body wards off disease and maintains health. Understanding this connection can empower individuals to make informed choices that bolster their immune defenses. The human gut, home to a vast array of microorganisms, plays a pivotal role in shaping the immune system’s responses.
The Role of the Gut in the Immune System
Approximately 70% of the body’s immune cells reside in the gut-associated lymphoid tissue (GALT). This extensive network is strategically positioned to monitor and respond to pathogens that enter the body through the digestive tract. The gut serves as the first line of defense, with the intestinal epithelium acting as a physical barrier and the gut microbiome playing an active role in modulating immune responses.
According to a review published in Nature Reviews Immunology, the gut epithelium not only prevents pathogens from entering the bloodstream but also interacts closely with gut microorganisms to regulate immune homeostasis. This dynamic interplay ensures that the immune system can distinguish between harmful invaders and benign dietary antigens.
How Gut Health Influences Immunity and Inflammation
Gut health is intrinsically linked to immune function through the actions of the microbiome. The microbiome, a diverse community of bacteria, viruses, fungi, and other microbes, educates and influences the immune system in several ways:
- Modulation of Immune Responses: Beneficial gut bacteria, such as Lactobacillus and Bifidobacterium, produce short-chain fatty acids (SCFAs) like butyrate. These metabolites have anti-inflammatory properties, promoting the development of regulatory T cells that help to maintain immune tolerance and reduce the risk of chronic inflammation.
- Pathogen Resistance: The healthy gut microbiota competes with pathogenic microbes for nutrients and attachment sites on the intestinal lining. This competitive exclusion reduces the likelihood of infections and maintains a balanced immune response.
- Immune System Activation: Gut microbes can enhance the production of protective antibodies. For instance, certain B cell populations in the GALT are stimulated to produce immunoglobulin A (IgA), a crucial antibody that neutralizes pathogens and prevents them from adhering to and penetrating the gut lining.
Disruptions in the gut microbiome, such as those caused by poor diet, antibiotic use, or chronic stress, can lead to dysbiosis—a state of microbial imbalance. Dysbiosis has been linked to increased susceptibility to infections and the development of inflammatory conditions such as Inflammatory Bowel Disease (IBD), according to research published in The Lancet.
The Impact of a Healthy Gut on Preventing and Managing Diseases
Maintaining a balanced and diverse gut microbiome is crucial for both the prevention and management of various diseases. Here are some examples:
- Allergies and Autoimmune Diseases: Emerging evidence indicates that gut health in early life can influence the risk of developing allergies and autoimmune diseases. A study in Nature Medicine suggests that exposure to a diverse set of microorganisms during infancy can train the immune system to differentiate between harmless and harmful antigens, potentially reducing the risk of allergic and autoimmune conditions.
- Infectious Diseases: A robust gut microbiome contributes to enhanced resistance against gastrointestinal infections like Clostridium difficile. Furthermore, a healthy gut supports the production of antimicrobial peptides that can directly target and neutralize pathogens.
- Chronic Diseases: Dysbiosis has been implicated in the pathogenesis of chronic diseases such as type 2 diabetes, cardiovascular disease, and even certain cancers. According to a study in Cell Host & Microbe, an imbalance in the gut microbiota can promote systemic inflammation, a well-known risk factor for these conditions.
Improving gut health can have a cascading positive effect on overall immune function and disease prevention. Strategies to enhance gut health include:
- Dietary Fiber: Consuming a diet rich in fiber promotes the growth of beneficial bacteria that produce SCFAs, supporting both gut and immune health.
- Probiotics and Prebiotics: Probiotics, found in fermented foods like yogurt and kefir, introduce beneficial bacteria into the gut. Prebiotics, such as inulin and oligosaccharides found in foods like garlic and onions, feed these beneficial microbes.
- Stress Reduction: Chronic stress can negatively impact the gut microbiome. Practices such as mindfulness meditation and regular physical activity can help manage stress levels and support gut health.
By prioritizing gut health, individuals can optimize their immune system’s functionality, promoting resilience against infections and reducing the risk of chronic inflammation and related diseases. This interconnectedness highlights the importance of a holistic approach to health, recognizing the gut as a central player in maintaining immune balance and overall wellness.
Gut Health and Metabolic Functions
The intricate relationship between gut health and metabolic functions is an area of growing scientific interest. The gut, often referred to as the second brain, plays a crucial role in regulating various aspects of metabolism, including nutrient absorption, energy balance, and fat storage.
Connection Between Gut Health and Metabolism
Your gut is home to trillions of microorganisms collectively known as the gut microbiome. These microorganisms, including bacteria, fungi, and viruses, have a profound influence on your metabolic health. Research indicates that an imbalance in the gut microbiome—a state known as dysbiosis—can contribute to metabolic disorders such as obesity, type 2 diabetes, and non-alcoholic fatty liver disease (NAFLD). A balanced gut microbiome, conversely, can promote efficient metabolic functions and overall health.
Microbiome Diversity and Energy Harvesting
Diverse gut microbiota are essential for optimal metabolic health. A variety of bacterial species ensures that our gut can efficiently break down complex carbohydrates and fibers into short-chain fatty acids (SCFAs). These SCFAs, including butyrate, acetate, and propionate, are crucial for providing energy to the cells lining the gut and influence overall energy homeostasis.
Studies have shown that individuals with obesity tend to have a less diverse gut microbiome compared to those with a healthy weight. This decrease in diversity can lead to an increased capacity of the microbiota to extract energy from food, contributing to weight gain and metabolic dysfunction. For example, a study published in the Journal of Clinical Endocrinology & Metabolism found that gut microbiota from obese individuals were more efficient at harvesting energy from the diet, resulting in greater energy storage and adiposity.
Influence on Glucose Metabolism and Insulin Sensitivity
Gut health also plays a pivotal role in glucose metabolism and insulin sensitivity. Dysbiosis has been linked to impaired glucose tolerance and insulin resistance, key features of type 2 diabetes. Beneficial gut bacteria, such as Akkermansia muciniphila and Bifidobacterium, have been shown to improve glucose homeostasis and insulin sensitivity.
For instance, a groundbreaking study published in Nature Medicine revealed that supplementation with Akkermansia muciniphila improved insulin sensitivity and reduced inflammation in obese insulin-resistant individuals. This suggests that enhancing the abundance of specific beneficial bacteria could be a potential therapeutic strategy for metabolic disorders.
How Gut Bacteria Affect Weight Management and Metabolic Diseases
The influence of gut bacteria on weight management and metabolic diseases extends beyond energy extraction and glucose metabolism. Gut microbiota produce various metabolites that can affect appetite regulation, fat storage, and systemic inflammation.
Appetite Regulation and Satiety
Gut bacteria are involved in the production of appetite-regulating hormones, such as ghrelin and leptin. SCFAs produced by bacterial fermentation of dietary fibers stimulate the release of the satiety hormone peptide YY (PYY) and the appetite-suppressing hormone glucagon-like peptide-1 (GLP-1). These hormones communicate with the brain to regulate food intake and promote feelings of fullness.
Moreover, certain gut bacteria can influence the endocannabinoid system, which plays a role in appetite regulation and energy balance. By modulating the levels of endocannabinoids, the gut microbiome can impact hunger signals and ultimately affect weight management.
Fat Storage and Adiposity
Gut bacteria also affect the storage of fat in adipose tissue. For example, the presence of lipopolysaccharides (LPS), components of the cell walls of certain gut bacteria, can trigger systemic inflammation and promote fat accumulation. Elevated LPS levels, a hallmark of metabolic endotoxemia, are commonly observed in obese individuals and contribute to insulin resistance and adiposity.
In contrast, beneficial bacteria such as Bifidobacterium and Lactobacillus produce anti-inflammatory compounds that mitigate inflammation and support a healthy weight. These bacteria also enhance the integrity of the gut barrier, preventing the translocation of LPS into the bloodstream and reducing metabolic endotoxemia.
Tips for Maintaining a Healthy Gut for Optimal Metabolic Health
Maintaining a healthy gut is essential for optimizing metabolic health. Here are evidence-based tips to support a balanced gut microbiome and promote overall well-being:
1. Consume a Diverse and Fiber-Rich Diet
A diet rich in diverse plant-based foods provides the necessary fibers and polyphenols that nourish beneficial gut bacteria. Include a variety of fruits, vegetables, whole grains, legumes, nuts, and seeds to support microbiome diversity and produce SCFAs through fermentation.
2. Include Probiotic and Prebiotic Foods
Probiotics are live beneficial bacteria found in fermented foods such as yogurt, kefir, sauerkraut, kimchi, and kombucha. Prebiotics, on the other hand, are non-digestible fibers that serve as food for gut bacteria. Examples include garlic, onions, leeks, asparagus, and chicory root. Including both in your diet can help maintain a healthy balance of gut bacteria.
3. Avoid Excessive Use of Antibiotics
While antibiotics are essential for treating bacterial infections, their overuse can disrupt the gut microbiome by indiscriminately killing both harmful and beneficial bacteria. Use antibiotics judiciously and only when prescribed by a healthcare professional.
4. Manage Stress Levels
Chronic stress can negatively impact gut health by altering the composition of gut bacteria and increasing gut permeability. Engage in stress-reducing activities such as mindfulness meditation, yoga, regular physical exercise, and adequate sleep to support a healthy gut.
5. Stay Hydrated
Proper hydration is essential for maintaining the mucosal lining of the intestines, which supports the growth of beneficial bacteria. Aim to drink sufficient water throughout the day to promote gut health and overall metabolic function.
By following these tips and fostering a healthy gut microbiome, you can optimize your metabolic functions and support your broader health goals.
In conclusion, it is evident that the health of our gut extends far beyond its primary role in digestion. A deeper understanding of the gut reveals a complex and dynamic system that significantly influences various aspects of our overall health. The intricate connection between the gut and the brain, termed the gut-brain axis, underscores the profound impact gut health has on mental well-being. Emerging research continues to highlight how an imbalance in gut bacteria can contribute to mood disorders and cognitive impairments, further solidifying the need for maintaining a balanced gut microbiome to support mental health.
Similarly, the gut’s pivotal role in the immune system cannot be overstated. The gut acts as a crucial barrier and an active participant in immune response, with its health directly affecting our body’s ability to fend off pathogens and manage inflammation. A robust gut microbiome holds the potential to prevent and manage numerous diseases, emphasizing the importance of nurturing gut health as a cornerstone of preventive healthcare.
Furthermore, the interplay between gut health and metabolic functions illustrates another critical facet of the gut’s influence. Gut bacteria play a significant role in regulating metabolism, impacting everything from nutrient absorption to weight management and the risk of metabolic diseases. Practical steps towards maintaining a healthy gut, such as a balanced diet rich in fiber, probiotics, and prebiotics, can lead to optimal metabolic health and overall well-being.
The growing body of evidence points to the gut as a central hub that connects multiple bodily systems, reinforcing the value of a holistic approach to health. By prioritizing gut health, we unlock the potential for a healthier mind, a stronger immune system, and a more efficient metabolism—ultimately enhancing our quality of life.